On the cutting edge of cancer research with Associate Professor Shankar Siva
23 November 2022
SBS World News: Prostate cancer clinical trial delivers exciting results for patients SBS News
As the head of the Stereotactic Ablative Radiation Therapy (SABR) program at Peter Mac, Associate Professor Shankar Siva is helping lead the way in developing new, more effective treatments for those affected by cancer.
By taking advantage of the latest advances in technology and research into radiation therapy, A/Prof Siva and his team are determined to not only uncover new treatment strategies for cancer, but to also help improve a patient’s quality of life by delivering kinder and gentler treatments with far fewer side effects.
Thanks to donations like yours, A/Prof Siva has made significant strides in his research and is excited about the huge potential SABR presents in treating all cancers.
Supporters like you are an essential part of what makes cutting-edge research like this possible, and we are very proud to be sharing with you the ground-breaking work A/Prof Siva is doing in the fight against cancer.
Pioneering SABR at Peter Mac
Radiotherapy, or radiation therapy, is one of the most effective tools we have in the fight against cancer. As you may already know, radiotherapy treatments typically involve clinicians seeking to destroy or injure cancer cells by targeting them with precise, controlled doses of radiation.
However, one of the main difficulties in using radiotherapy for treatment is that radiation can be just as effective at harming normal, healthy cells as it is with cancer cells.
That’s why, for A/Prof Siva, one of the most exciting breakthroughs to happen in cancer research in the past decade is the development of SABR technology, he explains:
“Instead of long courses of radiotherapy that can last many weeks, SABR is a high precision, high dose radiation treatment that allows us to deliver the equivalent treatment effect in very short, compressed treatments.
"The main difference is that we can be far more accurate than we were before. We're talking about millimetre-to-millimetre accuracy in delivering the treatments. And that allows us to really ramp up the radiation treatment itself.”
Because SABR is much more accurate than conventional radiotherapy, it can deliver a much higher dose of radiation without damaging surrounding tissue.
SABR works by placing the patient in a specialised machine that takes a four-dimensional CT scan of their body to get a clear picture of where a patient’s tumour is located. The radiation therapy team then uses these scans to design a SABR treatment that’s completely unique to that specific patient.
From there, clinicians use the same machine to deliver several radiation beams from a variety of angles, each one precisely calibrated to target only the tumour and nothing else.
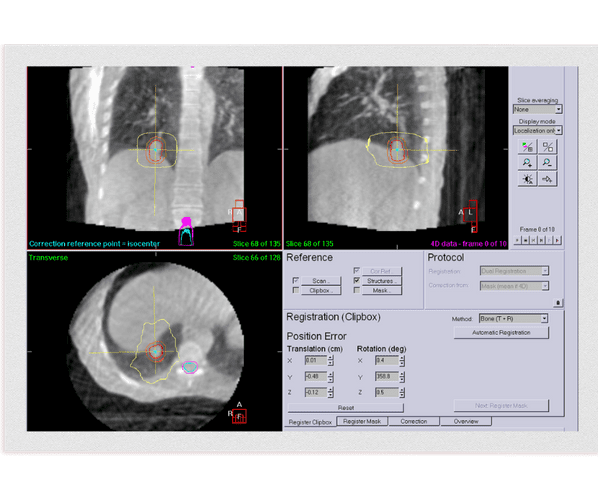 A CT scan is used to ensure that SABR treatment lines up exactly to the same point at every treatment session and remains that way throughout treatment delivery.
A CT scan is used to ensure that SABR treatment lines up exactly to the same point at every treatment session and remains that way throughout treatment delivery.
According to A/Prof Siva, thanks to its high degree of precision and accuracy, SABR treatments also often take much less time and produce fewer side effects than conventional radiotherapy.
Instead of having to come into the clinic every day over the course of several weeks to receive their radiotherapy treatment, patients who undergo SABR treatments typically only need to go through up to five treatments in total. All of this gives A/Prof Siva and his team real hope that SABR could become the new standard of care for radiotherapy in the near future.
“I think the future of radiation oncology could be these ultra-short treatments. Our results indicate that SABR can be a safe and effective treatment for patients whose cancer has spread to their lungs, even when it’s delivered in a single session.”
Combining SABR and immunotherapy
Recently, A/Prof Siva has been conducting clinical trials that combine the use of SABR with another recent ground-breaking discovery: immunotherapy.
Early results of this research have been very promising, with A/Prof Siva and his team discovering that SABR is not only effective at eradicating cancer cells, but it can also stimulate a person’s immune system at the same time.
“Immunotherapy is a major advance in cancer therapy, with the potential to improve outcomes in a range of different cancers. However, methods to improve the effectiveness of immunotherapy are urgently needed. This is where radiotherapy fits in.
"I hope my research will significantly benefit cancer patients by providing them with access to effective, precision SABR + immunotherapy treatment, as well as identifying patients who are most likely to respond to this treatment.”
Immunotherapy is a type of cancer treatment that boosts the body’s natural defences, helping your immune system fight cancer. It is one of the most exciting breakthroughs in cancer research in recent times, but it is still in its early stages of development and further research is needed to expand immunotherapy’s application for all cancer patients.
Thanks to research like A/Prof Siva’s and his team, we now know that in order to increase a patient’s chances of responding to immunotherapy, their immune system must be primed and ready to recognise the cancer cells. Which is exactly where SABR comes in.
“SABR breaks up some of the cancer cells and this allows the tumour specifically to be recognised by the immune system, allowing the white cells to mount an immune response. SABR is like a match to start the fire, and immunotherapy is the fuel that sustains the flame.”
These combined insights have led to further research and the development of new ‘combination therapies’ that use SABR and immunotherapy together.
SABR radiotherapy is used to attack the initial tumour, or clump of cancer cells, while also kick-starting an immune response to the tumour. Patients then go through a course of immunotherapy to ‘mop up’ any remaining cancer cells, with the aim of delaying the recurrence of cancer or eradicating it altogether.
 A/Prof Siva with some of the SABR team at Peter Mac
A/Prof Siva with some of the SABR team at Peter Mac
According to A/Prof Siva, research into this type of combination therapy has the potential to open many doors for designing kinder and gentler cancer treatments for those affected.
Most importantly though, for A/Prof Siva and the SABR team at Peter Mac, this new line of research also increases the treatment options available to those affected with cancer, especially for patients where surgery isn’t possible.
“Some patients simply can't undergo surgery. Maybe they've got an issue with their hearts or maybe they're on blood thinners or maybe their lungs are not up to it. And oftentimes, for these patients, they don't have many options because there's no alternative treatment. But now, what we're seeing with SABR is that it can be as good as, or better than, surgery in the first place.”
How research gives us the insights for new combined treatments
One very important point that A/Prof Siva is quick to mention is that as impressive and innovative as SABR technology is, the only reason it exists in the first place is because of the decades of research that had to happen first.
“First of all, research gave us new immunotherapy treatments. Then research showed us that SABR might be a way to improve patient response to immunotherapy.”
Advancements and breakthroughs such as these don’t happen in a vacuum, and A/Prof Siva is eager to continue building upon that foundation of knowledge.
Together with his team of radiation oncologists, clinicians, researchers, and medical physicists, A/Prof Siva is currently leading several international trials that aim to explore the potential for SABR to be used to treat and cure many different types of cancer.
“We’re leading trials on things like lung cancer, prostate cancer, there's a breast cancer trial, and even kidney cancer. So far what we've seen seems pretty promising, and we’re already expanding into a lot of different trial settings.”
For A/Prof Siva, it’s an exciting time for cancer research and he is very grateful to be able to conduct his research at Peter Mac.
Not only is Peter Mac the home to Australia’s first SABR clinic and other cutting-edge technologies, Peter Mac is also Australia’s largest cancer research site with over 700 researchers, offering A/Prof Siva the unique opportunity to collaborate with a multitude of experts from a wide variety of fields.
This is both beneficial for patients and it also helps work like A/Prof Siva’s so that researchers can discover new treatments and cures more quickly.
“I think it's a really unique thing about Peter Mac because we house researchers alongside clinicians and it's an aspect that I wouldn't get access to if I were somewhere else. It would affect the way that I'd be able to conduct my research, because I don't think I'd have the same level of insight and I don't think I'd have the same level of collaboration if I weren’t at Peter Mac.
"You’ve got lab researchers developing fundamental knowledge of cancers, working with translational researchers who can translate those insights into potential therapies. Then clinical researchers like me take those therapies and try to maximise the effect in patients.”
Thank you for your support

A/Prof Siva is just one of the many talented researchers at Peter Mac whose work is made possible through support like yours, something he is extremely grateful for.
Read A/Prof Siva's message to Peter Mac supporters below:
“We wouldn't be able to make the advances in cancer cures and treatments without donor support for research. Having the community pitch in to help us develop and accelerate cancer cures is such an important way to help us move forward.
Research like this is of critical importance because it means we can develop and accelerate cancer cures. This is the best way to move forward with cancer breakthroughs in the future."
@Follow us on Instagram (@SupportPeterMac)







