Unlocking the secrets of kidney cancer
5 min read 28 June 2024
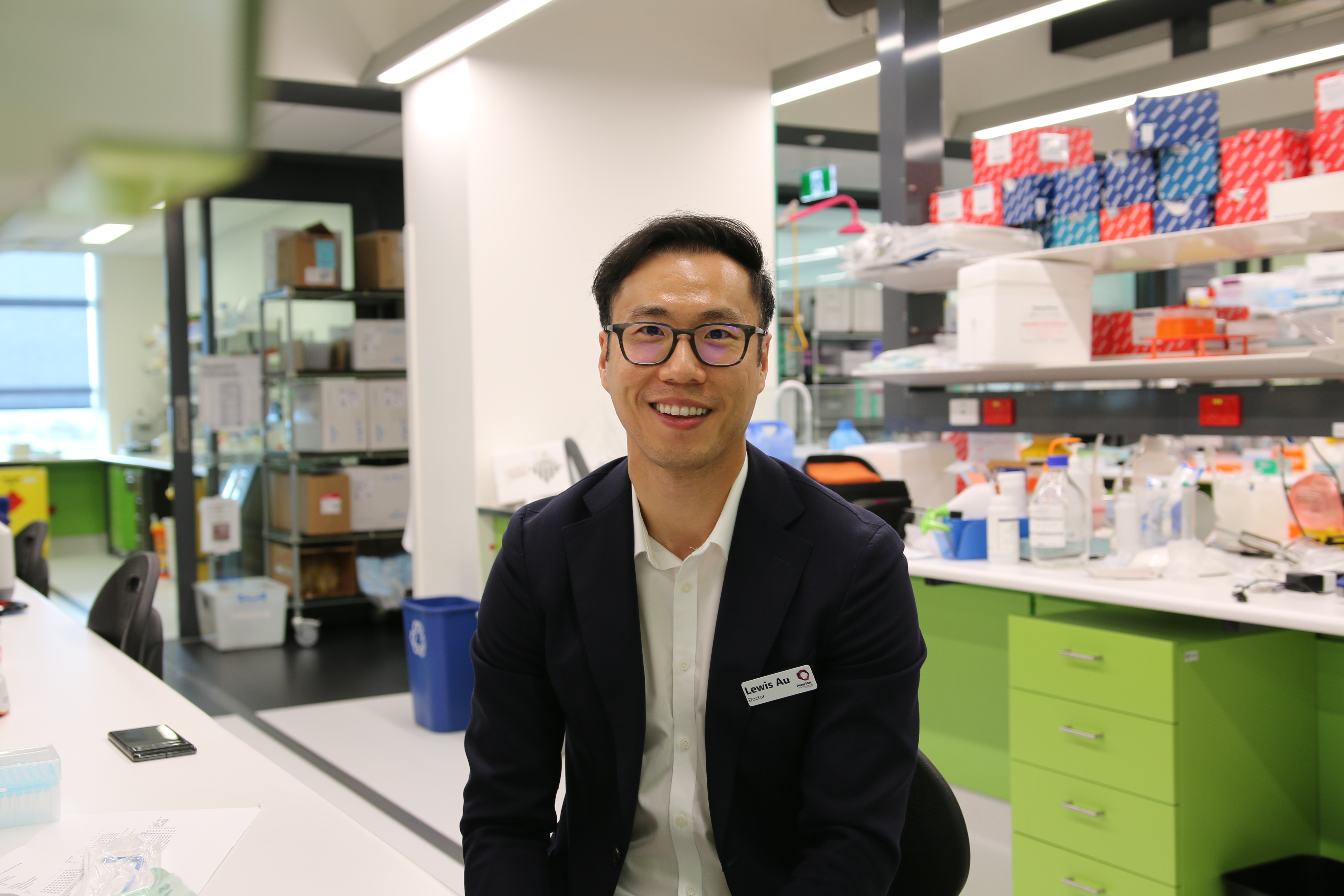
Dr Lewis Au explains how receiving a Discovery Partner Fellowship from Peter MacCallum Cancer Foundation will help take his discoveries from the research laboratory to the patient bedside, transforming treatment for people with kidney cancer.

It’s the time he spends in the clinic that gives medical oncologist Dr Lewis Au a “fire in the belly”.
“The days that I sit with patients having discussions about treatments – that’s what drives me to do more in the research setting.”
Lewis’s journey began in London where he worked as a Clinical Fellow at leading cancer hospital, the Royal Marsden.
“Patients really want to know ‘Is that drug going to help me? Is it the right drug? How do I avoid drugs that will only give me side effects?’”
Determined to unlock the answers, Lewis undertook his PhD in Cancer Genomics and Tumour Immunology at the Francis Crick Institute in the UK. After five years abroad, investigating the impact of immunotherapy on kidney cancer, Lewis set his sights on returning home and continuing his work at Peter Mac.
“There was no other institute I wanted to work at back in Australia,” he says.
In 2022, Lewis joined Peter Mac working as a full-time medical oncologist caring for people with kidney cancer, balancing it with his Postdoc Research Fellow in Paul Neeson’s immunology lab.
Being a recipient of the Peter Mac Foundation’s 2023 Discovery Partner Fellowship will allow Lewis to dedicate more time to his vital work.
Translating research into patient care
Translating research into tangible outcomes for patients is where Lewis finds his work most rewarding.
“Peter Mac has this incredible track record of supporting translational research”, he says.
“It’s so unique that it’s an integrated institution of patient care and cancer research – practically, and in culture as well. The institute has seven levels of clinical care and then you've got the direct interface with the lab. That, to me, is the most efficient way to advance cancer care and get fundamental findings to patients in the most streamlined way.”
Lewis explains how translational research can be divided into two aspects – backward translation, and forward translation.
“Backward translation is about taking observations in the clinic to the lab and trying to understand the biological underpinnings of the disease - how the disease works, how the treatment works. All treatments start from a fundamental understanding of the biology behind it.”
“Then we have forward translation, which is about taking that fundamental understanding to develop an intervention – a new treatment, drug, or test – and bringing it back to the clinic.”
“That cycle is how we advance life sciences, and in particular, cancer research.”
Lewis’s project is using a fundamental understanding of immunotherapy and its challenges, and taking the next steps to identify signals that will help provide tailored treatments for patients with kidney cancer.

A complicated cancer
“Kidney cancer is a reasonably uncommon cancer,” Lewis says.
“For a long time it has been a neglected disease in terms of research. Not many therapies have worked, but immunotherapy in the last five to 10 years has transformed the therapeutic landscape.”
But there are challenges in ensuring immunotherapy is used correctly. While about 50 per cent of patients with kidney cancer will benefit from immunotherapy, the other half won't.
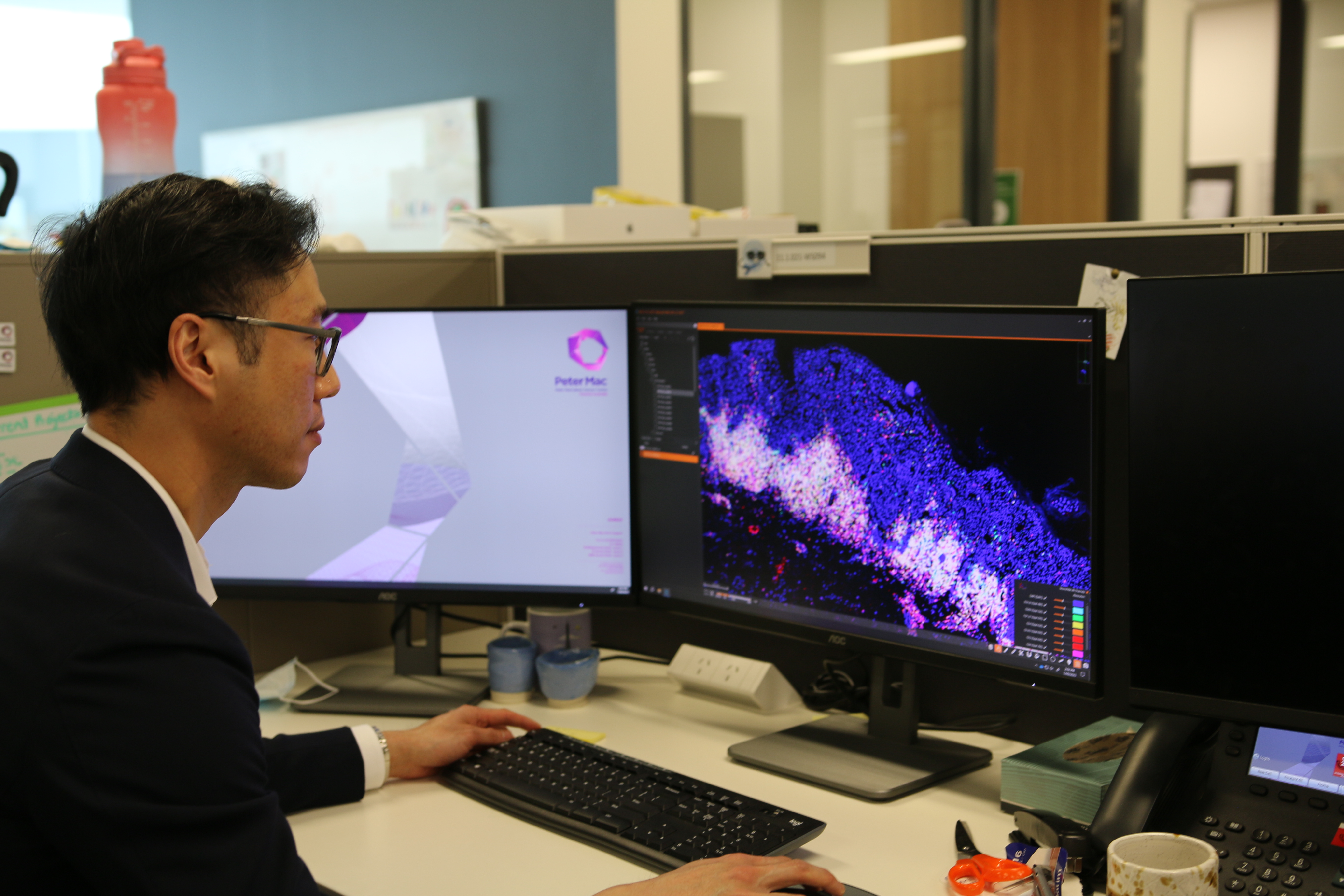
Lewis explains that solid cancers like kidney cancer are highly heterogeneous – meaning, they are made up of very different populations of cancer cells.
“Kidney cancers are almost like a mosaic – it is just so busy and different in every single part. If you take a sample from one area of a kidney cancer, your results might be different to another sample from another area. This makes testing or developing a clinical assay very difficult.”
Kidney cancers can also grow to about 13cm, equating to hundreds of billions of cells. As cancers grow, different populations of cancer cells emerge, further complicating diagnostic testing limited to a single needle biopsy.
“Doing multiple biopsies for a patient is not practical, which is one of the reasons there have not been any biomarkers in clinics for kidney cancers at all”, says Lewis.
“My project is about trying to find a biomarker that isn’t subject to heterogeneity - where a single biopsy will be representative of the patient’s whole tumour - and using that information to predict immunotherapy outcomes.”
Finding the ‘holy grail’
Personalising treatments for patients with kidney cancer is Lewis’s ultimate goal.
Discovering a biomarker will help Lewis and his team develop a test to predict cases where treatment will be ineffective, helping to reduce overtreatment and reduce side effects.
“What I'm interested in is to see whether it is feasible to find this holy grail biomarker — where one biopsy is enough to tell if a patient will respond to immunotherapy or not.”
While progress has been made to identify some molecular markers, such as RNA or gene expression as potentially useful, researchers haven’t yet been able to translate this into patient care.
Lewis is leveraging his previous work using an RNA-based test to find out what the signature is for kidney cancer and how this relates to immunotherapy response.

Taking it to the next level
Once a biomarker is identified, Lewis aims to validate the findings using materials collected by national kidney cancer registry and biobank, KRAB – a collaborative project that collects clinical data and biospecimens to support a broad range of research and education initiatives.
The patient samples and analysis will then be done jointly between Peter Mac and colleagues at the Francis Crick Institute in the UK.
“This research is a continuation of the work I started in the UK”, Lewis says. “The project is a collaboration between two world-leading institutes.”
“Bringing additional collaborators on board is really important. There's additional expertise and ideas that come because of collaborative processes. I think this is how we can advance the field. It's not a single researcher, it's about a team.”
“My long term aspiration is to develop a test that can help clinicians provide better advice on which treatment to use for specific patients” says Lewis.
“A problem we face is that a lot of research assays are not techniques we can apply to the clinic. Often they’re too complicated to be applied at scale. They might also be too expensive to bring to the bedside.”
“The aim is to develop a test that is suitable for clinical implementation we can use in the clinic, not just the labs, helping to bring personalised treatment to all patients, everywhere.”
 Lewis pictured with colleagues from his lab at the Francis Crick Institute in the UK
Lewis pictured with colleagues from his lab at the Francis Crick Institute in the UK
Essential support
Lewis describes the Discovery Partner Fellowship as essential in allowing him to carve out more time to spend in the lab, which is a key aspect of advancing the research. It will also help him to build a team, including data analysts and research assistants.
“Funding for cancer research is vital”, he says.
“Research is expensive. The number of people and teams, and the resources required to advance the molecular understanding of cancer and to develop new tests, requires a huge amount of resources and manpower.”
This amount of work would not be possible without funding from Peter Mac’s Discovery Partners.
“This funding is helping cutting-edge research, and it's research that is very much close to the bedside. Peter Mac is at the forefront of cancer care, and I truly think that transformative treatments will come from this program.”
Our wonderful Discovery Partners make regular monthly donations to Peter Mac to fund life-changing research like Lewis's.
By donating to the Peter MacCallum Cancer Foundation, you can help other early or mid-career researchers like Dr Au continue their vital work to discover kinder, more effective treatments for people affected by cancer.
Become a Discovery Partner today
@Follow us on Instagram (@SupportPeterMac)







