Breakthroughs for bowel cancer: with Dr Oliver Piercey
5 min read 12 February 2024
Thanks to the kindness of the Peter Mac community, cancer research is moving at a pace never seen before. But sadly lives are still being lost. Dr Oliver Piercey is determined to change this by discovering breakthroughs for bowel cancer.
To understand Dr Piercey’s work, we need to understand what is known as the BRAF mutation.
A BRAF mutation is like a glitch in the BRAF gene. This rare and random genetic mutation causes cells to become several hundred times more active than normal cells, giving constant signals to cells to keep dividing without any instruction to stop. This can cause tumours to develop.
For cancers caused by a BRAF mutation, this fault acts like an accelerator for the cancer, urging it to keep growing.
“This is a normal protein that normally causes cell growth, but when this mutation happens, it turns the cell very active, and it makes it about 700 times more active than a normal cell. And it keeps growing and growing and dividing and dividing,” says Dr Piercey.
Accelerating research into BRAF mutations and personalised treatments
It is reassuring to know that cancer research in the past has led to progress in treating some cancers caused by the BRAF mutation, such as BRAF-mutant melanoma. But challenges remain with other types of cancer, such as BRAF-driven bowel cancer. These past discoveries give Dr Piercey the determination to take on these challenges.
"In 2024, I am excited to be working on several projects focusing on BRAF-mutant metastatic bowel cancer," he shares.
“Firstly, we aim to improve our understanding of which features within a tumour can predict the chance of a patient’s response to targeted therapy. This could help us work towards providing a more individualised treatment plan for patients.”
Rather than treating all patients the same, it’s important that we look at each patient’s tumour in detail, and then consider what’s going to be the most effective option for them.
“In the case for a patient who we identify has the BRAF mutation, instead of just giving them standard chemotherapy treatment, they can receive treatment that’s targeted to this underlying mutation, which is driving their cancer. This is a personalised therapy,” Dr Piercey shares.
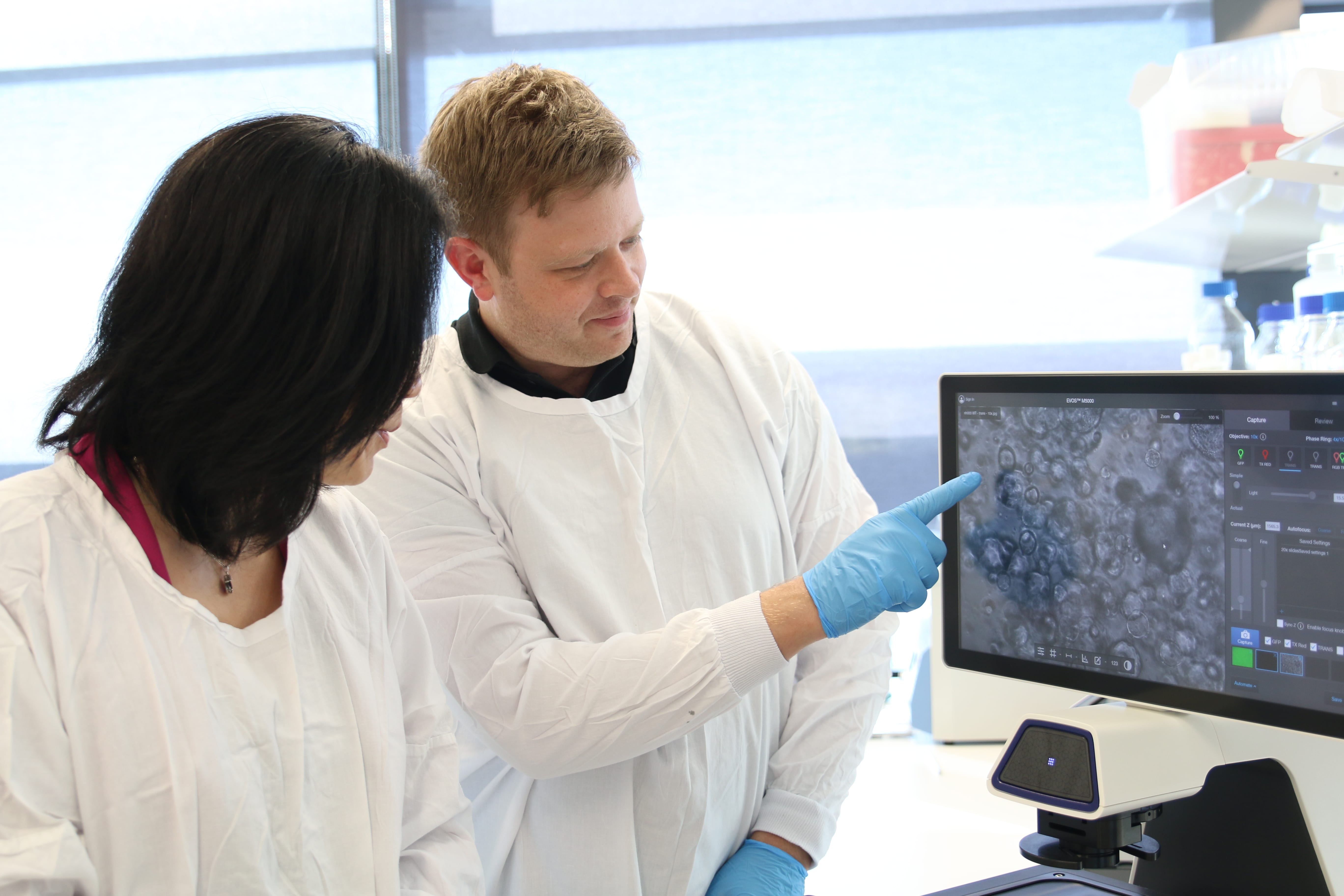
In the lab, Dr Piercey and his team will analyse tumour tissue samples from patients who have undergone these targeted therapies. Using advanced techniques like single-cell RNA sequencing, they aim to identify specific genetic features that can predict whether a patient will respond well or poorly to treatment.
This visionary approach sets the stage for the design of novel therapies, a critical step towards improving outcomes for patients facing this challenging cancer.
Tracking the timeline of treatment resistance
Another key research goal of Dr Piercey’s is to understand more about what causes treatment resistance in BRAF-mutant bowel cancer patients, and the role the immune system could play in overcoming this resistance. He says:
"We hope to gain a greater understanding of the mechanisms that evolve within tumours – mechanisms that can bypass the cancer-killing effect of our treatments.”
To better understand how to tackle treatment resistance, Dr Piercey and his team plan to analyse tumour tissue from patients both before and after the development of treatment resistance. This analysis will create a timeline of the disease's progression.
To achieve this, Dr Piercey plans to use patient-derived tumour organoids. Created from patient cells, these are lab-grown miniature replicas of tumours that offer researchers an in-depth look into how tumours adapt and evade treatment.
“We'll be analysing tissue at diagnosis, and then also looking at tissue in patients whose cancer has progressed despite their treatment. Then we’ll compare the changes that occur at the genetic level between the two.
“We take the tumour sample from the lab and we extract the RNA. RNA is like the messenger for DNA, and it tells us what genes are turned on in the tumour at the time. What we’re trying to find out is what those cells are doing that allow them to grow and to behave aggressively despite the treatment they’re receiving,” says Dr Piercey.
With comprehensive profiling, Dr Piercey and his team will gain an in-depth understanding of the pathways activated within BRAF-mutant tumours to avoid being effectively treated. They hope that this knowledge will pave the way for the design of new therapies and treatment options for many more cancer patients in the future.
Thank you for your support
Your support for Peter Mac’s research is vital to these ground-breaking projects, and brings us one step closer to a future where no one will lose their life to cancer.

Dr Piercey wishes to extend his heartfelt gratitude to those who help make his work at Peter Mac possible:
Read Dr Piercey's message to Peter Mac supporters below:
"As a researcher, I wholeheartedly recognise that without our generous supporters, our mission would be an insurmountable challenge.
"Donations enable us to stride towards improving the lives of patients battling cancer. Without funding, research cannot progress and so we are extremely grateful for contributions, no matter the size. Thank you!"