Unlocking powerful new insights in lung cancer
4 min read 24 November 2025
November is Lung Cancer Awareness Month. We are pleased to spotlight some of Peter Mac’s pioneering research into lung cancer – one of the most common and deadly types of cancer.
Lung cancer remains one of Australia’s most devastating diseases. It was the fifth most commonly diagnosed cancer in 2024 and by the age of 85, one in 21 Australians is at the risk of a lung cancer diagnosis.
Professor Steven Stacker, a leading Peter Mac researcher who runs the Steven Stacker Lab, is determined to change this. His lab focuses on understanding how tumour cells can help cancer to grow and spread. Using world-class technology and cutting-edge techniques, Prof Stacker and his team aim to improve treatment and care for people diagnosed with primary or secondary lung cancer.
 Professor Steven Stacker (pictured) is leading research to understand how tumour cells enable both primary and secondary lung cancer
Professor Steven Stacker (pictured) is leading research to understand how tumour cells enable both primary and secondary lung cancer
Uncovering how lung cancer outsmarts treatment
For many people with lung cancer, chemotherapy is the first and most important line of defence. But over the course of treatment, some tumour cells learn to adapt and survive, making chemotherapy less effective. Known as chemotherapy resistance, this is one of the biggest obstacles in lung cancer treatment.
“When resistance happens, cancer can return or continue to grow,” explains Prof Stacker.
“This leaves lung cancer patients with fewer treatment options and worsening outcomes.”
To address this, Prof Stacker and Postdoctoral Researcher Dr Aadya Nagpal are following the trajectory of individual lung cancer cells as they undergo chemotherapy. By ‘tagging’ and tracking the cells, they can watch resistance as it happens.

“This gives us something we have never had before: a map of when and where chemotherapy resistance begins,” says Dr Nagpal.
The team has also identified a protein called RYK, which appears to play a powerful role in helping lung cancer cells resist chemotherapy. Excitingly, the Stacker laboratory has developed the world’s first tools that target cancer cells producing RYK. Combining these tools with advanced research techniques, the Stacker lab aims to uncover exactly how RYK enables chemotherapy resistance by watching it unfold in real-time. This approach has the potential to eliminate the tumour cells that produce RYK.
 How chemotherapy resistance occurs in primary lung cancer
How chemotherapy resistance occurs in primary lung cancer
Bad seeds: protecting the lungs from metastatic cancer
Cancers that begin in other parts of the body can also invade the lungs through a process called metastasis, causing secondary lung cancer. This is when cancer cell “seeds” detach from their original site – for example the breast, colon or kidney – and travel through blood and lymphatic vessels before taking root like an invasive weed in the “soil” of another organ.
Unfortunately, the lungs are particularly vulnerable, with up to 50% of patients with metastatic cancer developing secondary lung tumours over the course of their disease.
Prof Stacker and Senior Postdoctoral Research Officer Dr Rae Farnsworth are seeking to understand how primary tumours in other organs prepare the lungs for “seeding” by cancer cells.
“Primary tumours can create small environments in lungs through harmful immune responses and altering blood vessels, making lungs more susceptible,” says Dr Farnsworth.
 Dr Rae Farnsworth (centre) and the Stacker Lab Team are researching how to protect the lungs from cancer spread
Dr Rae Farnsworth (centre) and the Stacker Lab Team are researching how to protect the lungs from cancer spread
To better understand this, the Stacker lab focusses on endothelial cells, which line blood vessels and help control what moves from the bloodstream into the lung tissue. The team has so far made a fascinating discovery: not only are endothelial cells are the 'first responders', but they also appear to protect lungs against tumour cell invasion.
“Essentially, endothelial cells are the lungs’ secret guardians against metastasis,” says Dr Farnsworth.
The Stacker lab is now exploring ways to aid endothelial cells in preventing cancer from spreading to the lung. The team is also developing approaches to detect early changes to blood vessels. This could identify patients at high risk of developing secondary lung tumours, so that they may be treated sooner rather than later.
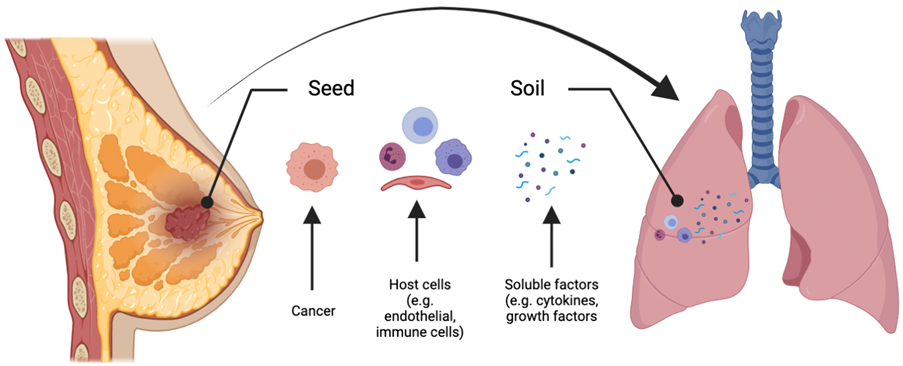 How tumour cells spread into the lungs, causing secondary lung cancer
How tumour cells spread into the lungs, causing secondary lung cancer
Transforming the future of lung cancer treatment
Understanding resistance and invasion is the key towards developing more effective, longer-lasting treatments for lung cancer. Peter Mac researchers like Prof Stacker, Dr Nagpal and Dr Farnsworth are closer than ever to making breakthroughs that can help more people survive this terrible disease.
Thank you to all Peter Mac supporters. Your generosity creates hope for improved outcomes, more options and more time for people affected by cancer.
@Follow us on Instagram (@SupportPeterMac)







